Introduction
Thyroid gland functions and disorders: The thyroid gland, a butterfly-shaped organ located at the base of the neck, is crucial for regulating the body’s metabolism, growth, and development. Through the secretion of thyroid hormones, this small gland influences nearly every organ system in the body. Understanding the anatomy, function, common disorders, and available treatments for thyroid-related conditions is essential for maintaining overall health and well-being.
Anatomy and Function of the Thyroid Gland
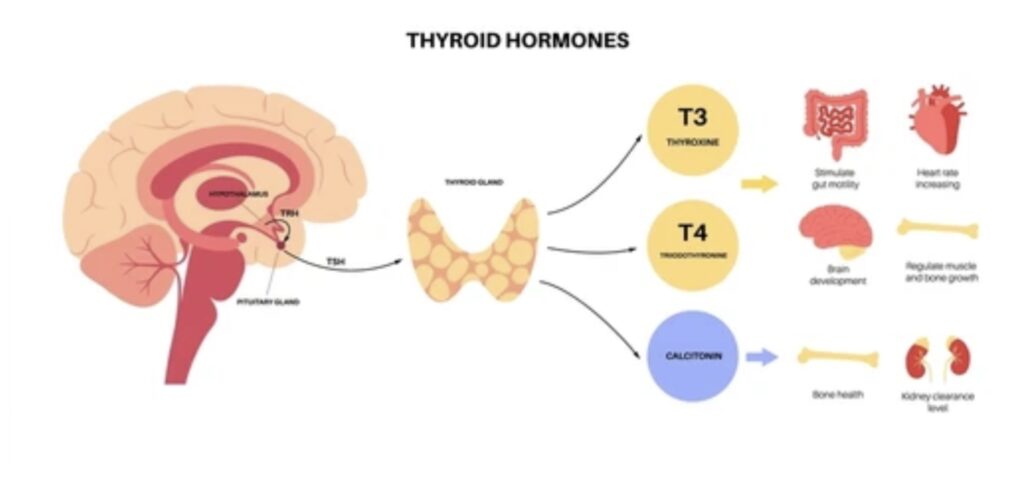
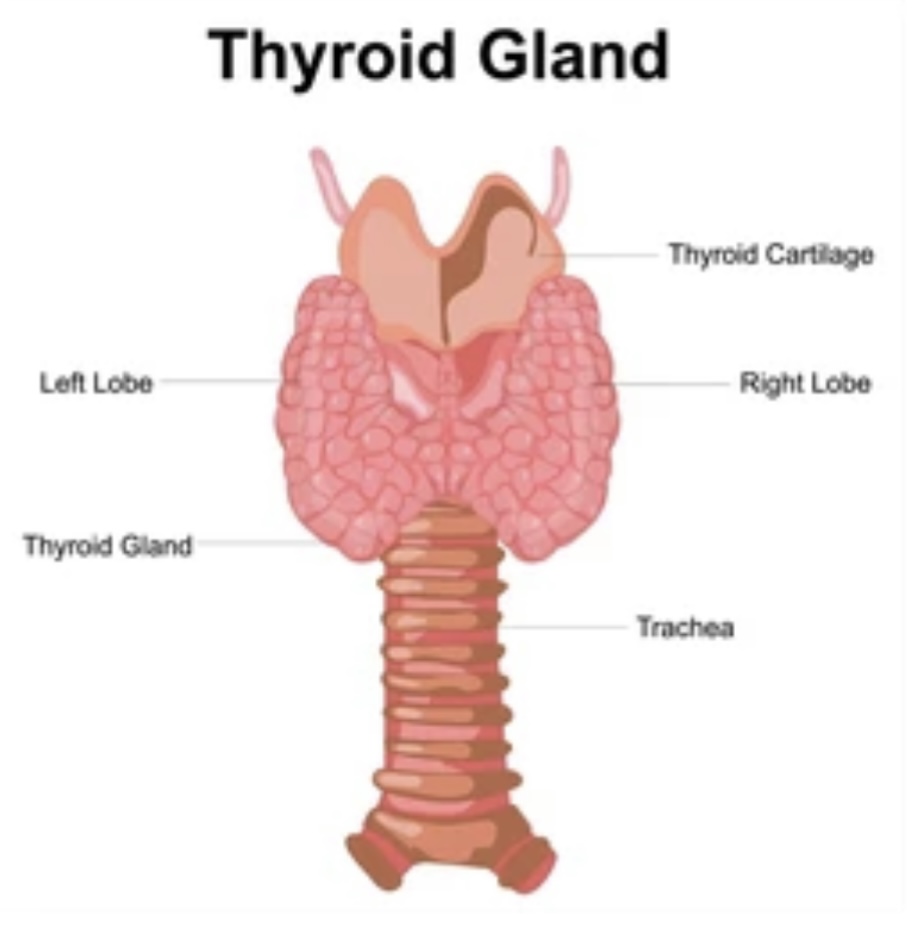
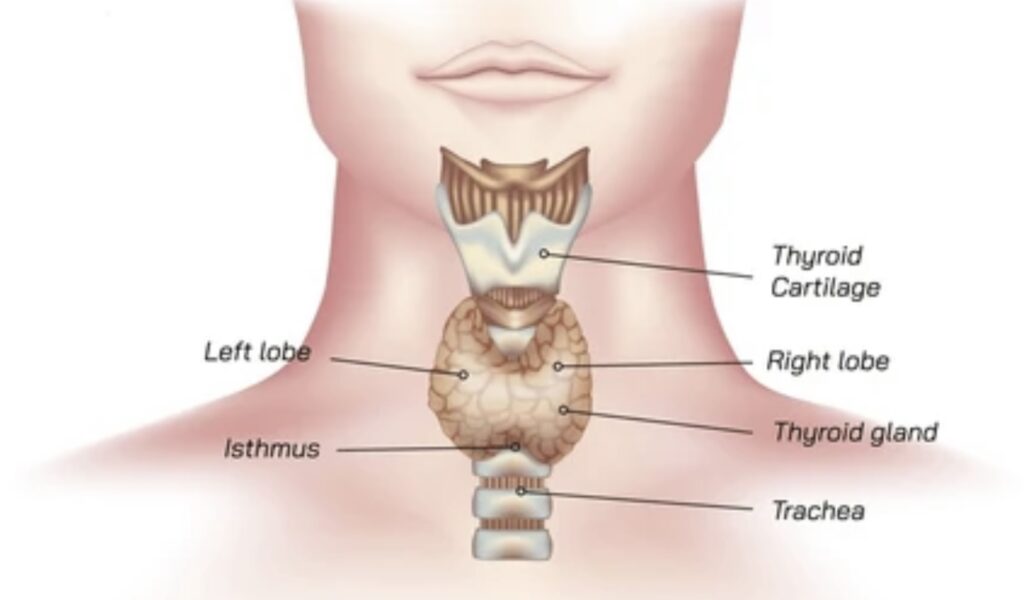
The thyroid gland is positioned in the front of the neck, just below the Adam’s apple, and consists of two lobes connected by a narrow band of tissue called the isthmus. It plays a pivotal role in the endocrine system, primarily by producing three key hormones: thyroxine (T4), triiodothyronine (T3), and calcitonin.
- Thyroxine (T4) and Triiodothyronine (T3): These hormones are synthesized from iodine and tyrosine, and they are essential for regulating the body’s metabolism. T4 is the more abundant hormone, but T3 is the more active form. Once released into the bloodstream, T4 is converted into T3 in various tissues, where it influences metabolic rate, heart function, digestion, muscle control, brain development, and bone health.
- Calcitonin: This hormone plays a minor role in calcium and phosphate metabolism. It works to lower blood calcium levels by inhibiting bone resorption and promoting calcium excretion in the kidneys.
The production and release of T4 and T3 are tightly regulated by the hypothalamus and pituitary gland through a feedback loop. The hypothalamus secretes thyrotropin-releasing hormone (TRH), which stimulates the pituitary gland to release thyroid-stimulating hormone (TSH). TSH, in turn, stimulates the thyroid gland to produce and release T4 and T3. When sufficient levels of thyroid hormones are present in the blood, they signal the hypothalamus and pituitary to reduce TRH and TSH production, maintaining a delicate hormonal balance.
Common Thyroid Disorders
Thyroid disorders are among the most common endocrine problems, affecting millions of people worldwide. These disorders can result in either overproduction or underproduction of thyroid hormones, leading to a range of health issues. The most common thyroid disorders include hypothyroidism, hyperthyroidism, thyroid nodules, and thyroid cancer.
1. Hypothyroidism
Hypothyroidism occurs when the thyroid gland fails to produce enough thyroid hormones. This condition can be caused by several factors, including autoimmune diseases (such as Hashimoto’s thyroiditis), iodine deficiency, certain medications, and surgical removal of the thyroid gland.
Symptoms of hypothyroidism can vary widely but often include fatigue, weight gain, cold intolerance, dry skin, hair loss, constipation, and depression. If left untreated, hypothyroidism can lead to more severe complications, such as heart disease, infertility, and in extreme cases, myxedema coma, a life-threatening condition.
The diagnosis of hypothyroidism is typically confirmed through blood tests that measure levels of TSH and T4. Elevated TSH and low T4 levels are indicative of an underactive thyroid.
2. Hyperthyroidism
Hyperthyroidism, the opposite of hypothyroidism, occurs when the thyroid gland produces too much thyroid hormone. The most common cause of hyperthyroidism is Graves’ disease, an autoimmune disorder where the immune system mistakenly attacks the thyroid, causing it to overproduce hormones. Other causes include toxic nodular goiter and thyroiditis.
Symptoms of hyperthyroidism include weight loss, rapid or irregular heartbeat, nervousness, irritability, tremors, excessive sweating, and heat intolerance. In some cases, patients may also develop a noticeable swelling at the base of the neck, known as a goiter.
Like hypothyroidism, hyperthyroidism is diagnosed through blood tests that show low TSH and high T4 or T3 levels. Additional tests, such as thyroid scans or radioactive iodine uptake tests, may be used to determine the cause of the condition.
3. Thyroid Nodules
Thyroid nodules are growths or lumps that can form within the thyroid gland. While most nodules are benign and asymptomatic, some can produce excess thyroid hormones, leading to hyperthyroidism. In rare cases, nodules may be cancerous.
Thyroid nodules are often discovered during routine physical exams or imaging studies performed for other reasons. To determine if a nodule is benign or malignant, doctors may perform a fine-needle aspiration biopsy, ultrasound, or thyroid scan.
4. Thyroid Cancer
Thyroid cancer is relatively uncommon but is one of the most treatable forms of cancer if detected early. There are several types of thyroid cancer, including papillary, follicular, medullary, and anaplastic thyroid cancer, each with different prognoses and treatment approaches.
Symptoms of thyroid cancer may include a lump in the neck, difficulty swallowing, hoarseness, and swollen lymph nodes. However, many cases are asymptomatic and are detected through imaging studies or biopsies of thyroid nodules.
Treatment Options for Thyroid Disorders
The treatment for thyroid disorders depends on the specific condition, its severity, and the patient’s overall health. Here are the primary treatment options:
1. Medication
- Hypothyroidism: The standard treatment for hypothyroidism is daily thyroid hormone replacement therapy, usually in the form of synthetic levothyroxine (T4). This medication restores normal hormone levels, alleviating symptoms and preventing complications. Regular monitoring of TSH levels is essential to ensure the correct dosage.
- Hyperthyroidism: Treatment for hyperthyroidism may involve antithyroid medications, such as methimazole or propylthiouracil, which reduce thyroid hormone production. Beta-blockers may also be prescribed to manage symptoms like rapid heart rate and tremors.
2. Radioactive Iodine Therapy
Radioactive iodine therapy is a common treatment for hyperthyroidism, particularly in cases caused by Graves’ disease or toxic nodular goiter. The patient takes a radioactive iodine capsule or liquid, which is absorbed by the thyroid gland, destroying overactive thyroid cells. This treatment often results in hypothyroidism, requiring subsequent hormone replacement therapy.
3. Surgery
Surgical removal of the thyroid gland (thyroidectomy) may be necessary for certain cases of hyperthyroidism, large goiters, or thyroid cancer. Depending on the extent of the surgery, patients may require lifelong thyroid hormone replacement therapy.
- Partial Thyroidectomy: Involves removing part of the thyroid gland. This may be done to treat benign nodules, cysts, or a localized thyroid cancer.
- Total Thyroidectomy: The complete removal of the thyroid gland is usually performed in cases of thyroid cancer or severe hyperthyroidism. After surgery, patients will need to take thyroid hormone replacement for life.
4. Monitoring and Lifestyle Changes
For mild thyroid disorders, particularly small benign nodules or subclinical hypothyroidism, doctors may recommend regular monitoring without immediate treatment. Patients are encouraged to maintain a healthy diet rich in iodine, engage in regular physical activity, and avoid smoking, which can exacerbate thyroid problems.
Conclusion
The thyroid gland, though small, has a profound impact on the body’s metabolic processes and overall health. Thyroid disorders, whether due to underproduction or overproduction of thyroid hormones, can lead to significant health challenges. However, with proper diagnosis, effective treatment options, and ongoing management, individuals with thyroid conditions can lead healthy and fulfilling lives. Advances in medication, surgery, and diagnostic techniques continue to improve outcomes for patients, underscoring the importance of early detection and tailored treatment plans for thyroid disorders.
Discover more from ZOOLOGYTALKS
Subscribe to get the latest posts sent to your email.


Pingback: HORMONES: CHEMICAL MESSENGERS | ZOOLOGYTALKS | 2024